Moist Wound Healing: Why Keeping Wounds Moist Is Better Than Dry Healing?
Moist Wound Healing: Why Keeping Wounds Moist Is Better Than Dry Healing?
Quick Summary
Is it better to let a wound dry out or keep it moist?
Unlike the traditional method where wounds are left open to form scabs, this “dry healing” approach often leads to several problems:
- Increased Pain – Scabs pull on underlying tissue and expose nerve endings, making dressing changes uncomfortable.
- Delayed Healing – A dry surface slows down cell migration and tissue regeneration, extending recovery time.
- Higher Risk of Scarring – Rigid scabs promote uneven skin repair, increasing the chance of hypertrophic or visible scars.
In contrast, moist wound healing maintains an optimal microenvironment. This prevents tissue dehydration, encourages cell migration, and promotes the natural release of growth factors essential for tissue repair.
What is Moist Wound Healing?
Moist wound healing is a revolutionary approach in modern wound care. First introduced by Dr. George D. Winter in 1962, research demonstrated that wounds heal up to 40% faster when kept moist compared to leaving them dry and exposed. This paradigm shift has transformed both hospital wound management and home wound care practices.
Key Principles of Moist Wound Healing
- Moisture Retention – A balanced moist environment accelerates epithelialization.
- Thermal Stability – Dressings preserve warmth, which increases enzymatic and cellular activity.
- Bacterial Protection – A sealed environment lowers the chance of external contamination.
- Enhanced Oxygenation – Adequate gas exchange supports cell survival.
- Autolytic Debridement – Moisture enables the body to naturally soften and remove necrotic tissue.
Benefits of Moist Wound Healing
- Faster Healing – A study published in the Journal of Wound Care revealed that moist wound environments reduced healing time by 30–50% compared to dry healing.
- Reduced Pain – Moist dressings protect nerve endings, significantly lowering pain levels. Patients with burns or pressure injuries often report improved comfort within 24 hours.
- Lower Risk of Scarring – Moisture prevents hard scab formation, leading to smoother skin regeneration and reduced risk of hypertrophic scarring.
- Cost-Effective Care – Though advanced dressings may seem more expensive initially, fewer dressing changes and faster recovery reduce overall treatment costs.
- Improved Quality of Life – Hydrocolloid dressings are discreet, waterproof, and flexible—allowing patients to shower or continue daily activities without disruption.
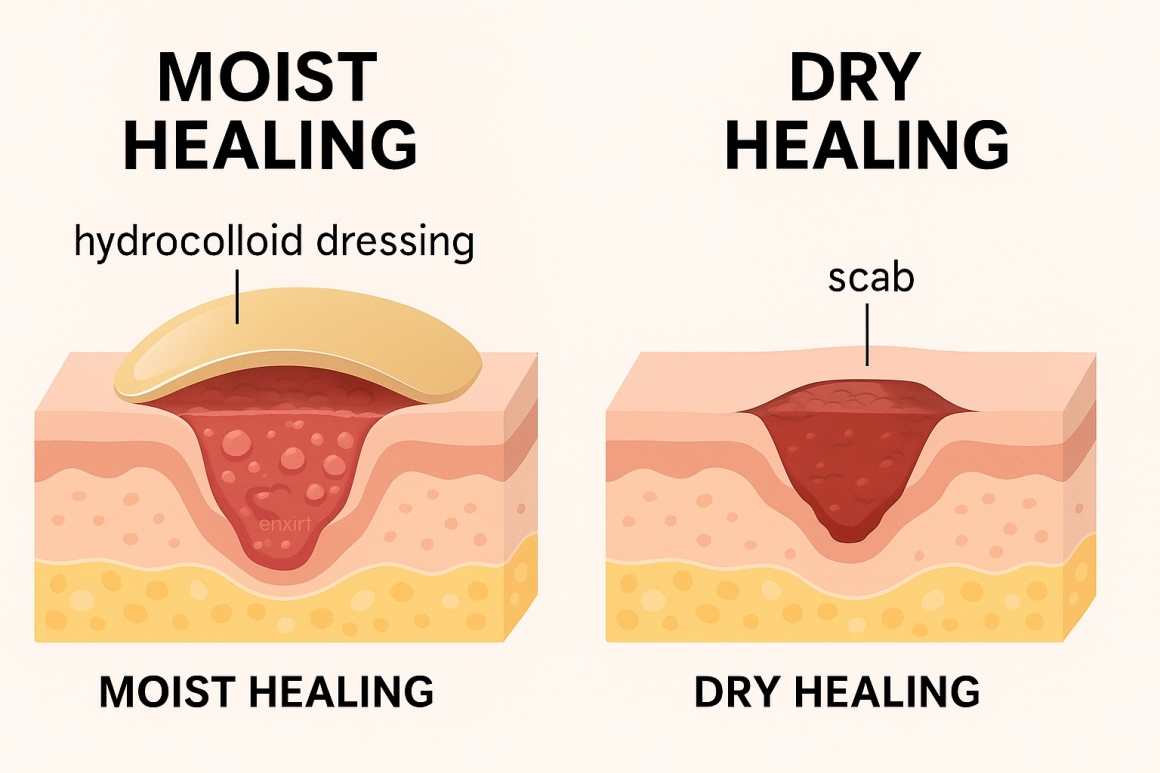
Moist vs. Dry Healing: A Comparison
Understanding the difference between Moist Wound Healing and traditional Dry Healing is critical for better wound care outcomes. The table below highlights key factors such as speed, pain level, scarring, and costs.
| Feature | Dry Healing (Traditional) | Moist Wound Healing (Modern) |
|---|---|---|
| Healing Speed | Slower | Faster (30–50% quicker) |
| Pain Level | Higher | Lower, more comfortable |
| Scar Risk | Higher | Reduced |
| Healing Environment | Open to air, forms scab | Closed, moisture-retentive |
| Common Materials | Gauze bandages | Hydrocolloid dressings, foam dressings, alginate dressings |
| Cost | Initially low, but higher long-term due to prolonged healing | Higher initial, but lower total cost thanks to quicker recovery |
The comparison shows why Moist Wound Healing is now considered the gold standard in wound care: faster recovery, reduced pain, fewer scars, and overall lower costs despite a slightly higher initial investment.

Hydrocolloid Dressings in Modern Moist Wound Care
Hydrocolloid dressings consist of gel-forming agents (such as carboxymethylcellulose, gelatin, and pectin) backed by a semi-permeable film. When applied, they interact with wound exudate to form a protective gel cushion. This maintains moisture balance while shielding the wound from friction and infection.
- Self-Adhesive & Easy to Apply – No secondary fixation required.
- Semi-Permeable – Blocks bacteria but allows oxygen exchange.
- Extended Wear Time – Can remain for 3–7 days, reducing frequent dressing changes.
- Non-Traumatic Removal – Protects fragile healing tissue during replacement.
- Maintain Optimal Moisture – Accelerates epithelialization and supports tissue regeneration.
- Protect Against Bacteria – Acts as a waterproof yet breathable barrier.
- Flexible and Discreet – Comfortable for use in hospitals, clinics, and at home.
The evidence is clear: adopting Moist Wound Healing with Hydrocolloid Dressings leads to faster recovery, less pain, and smoother skin remodeling compared to dry healing. Whether treating minor cuts at home or managing complex wounds in clinical settings, moist wound care is the gold standard in modern wound management.
More Articles
-
What Is a Hydrocolloid Dressing and How to Use It? Posted 2025-10-01